Anal papilla hypertrophy
OVERVIEW
What is hypertrophic anal papilla?
Hypertrophic anal papilla is a common anal condition, also known as anal papilloma or anal fibroepithelial polyp. It is a benign disease with a low potential for malignant transformation.
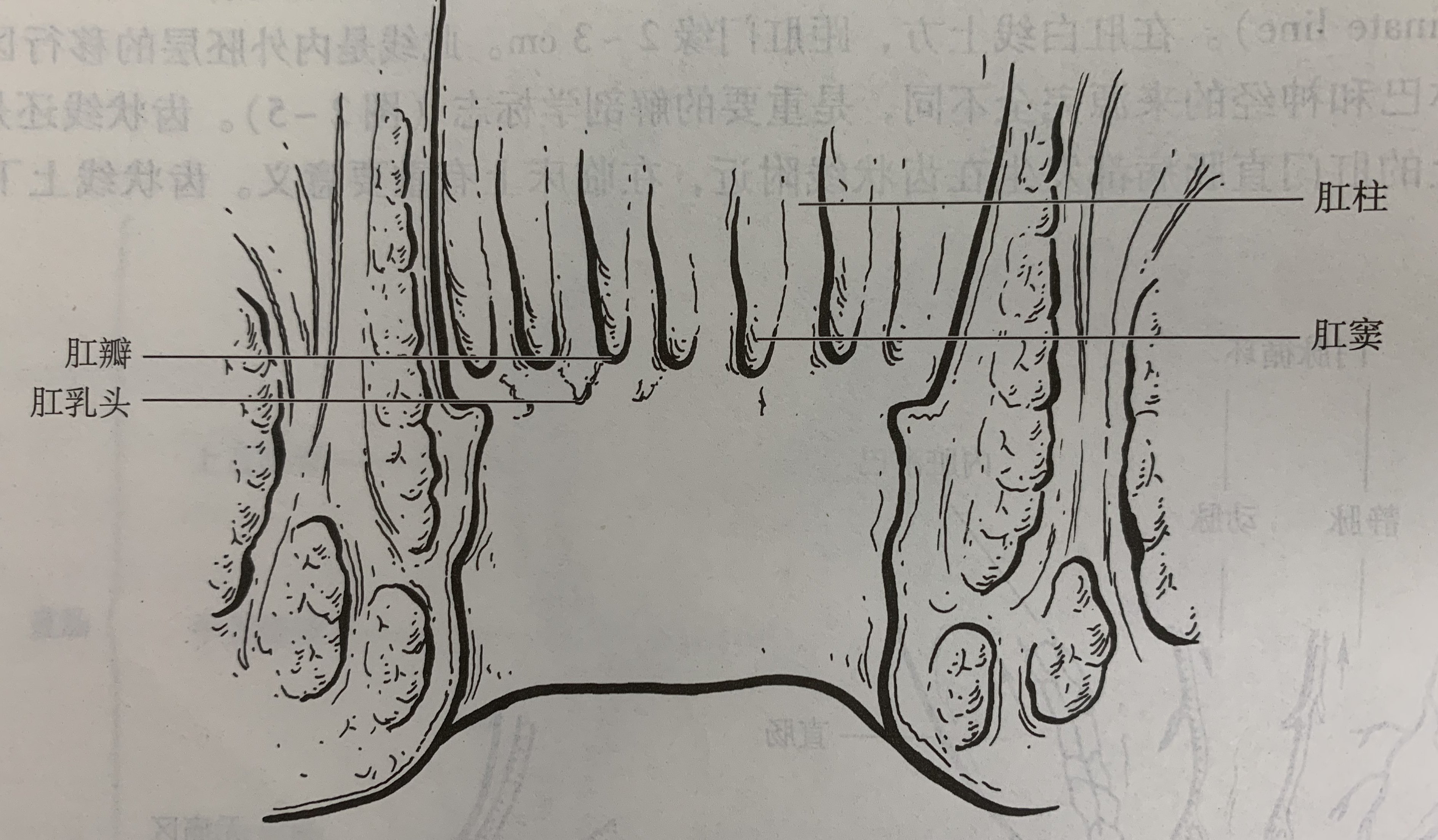
What is an anal papilla?
The anal papilla appears as a small triangular protrusion located at the lower end of the rectal columns, arranged along the dentate line in 2–6 formations. The base is reddish, while the tip is grayish-white, measuring 0.1–0.3 cm in height. When hypertrophied, it can reach 1–2 cm. The anal papilla consists of fibrous connective tissue, contains capillary lymphatics, and is covered by skin. The occurrence rate of anal papillae is 13%–47%, with most people not having them.
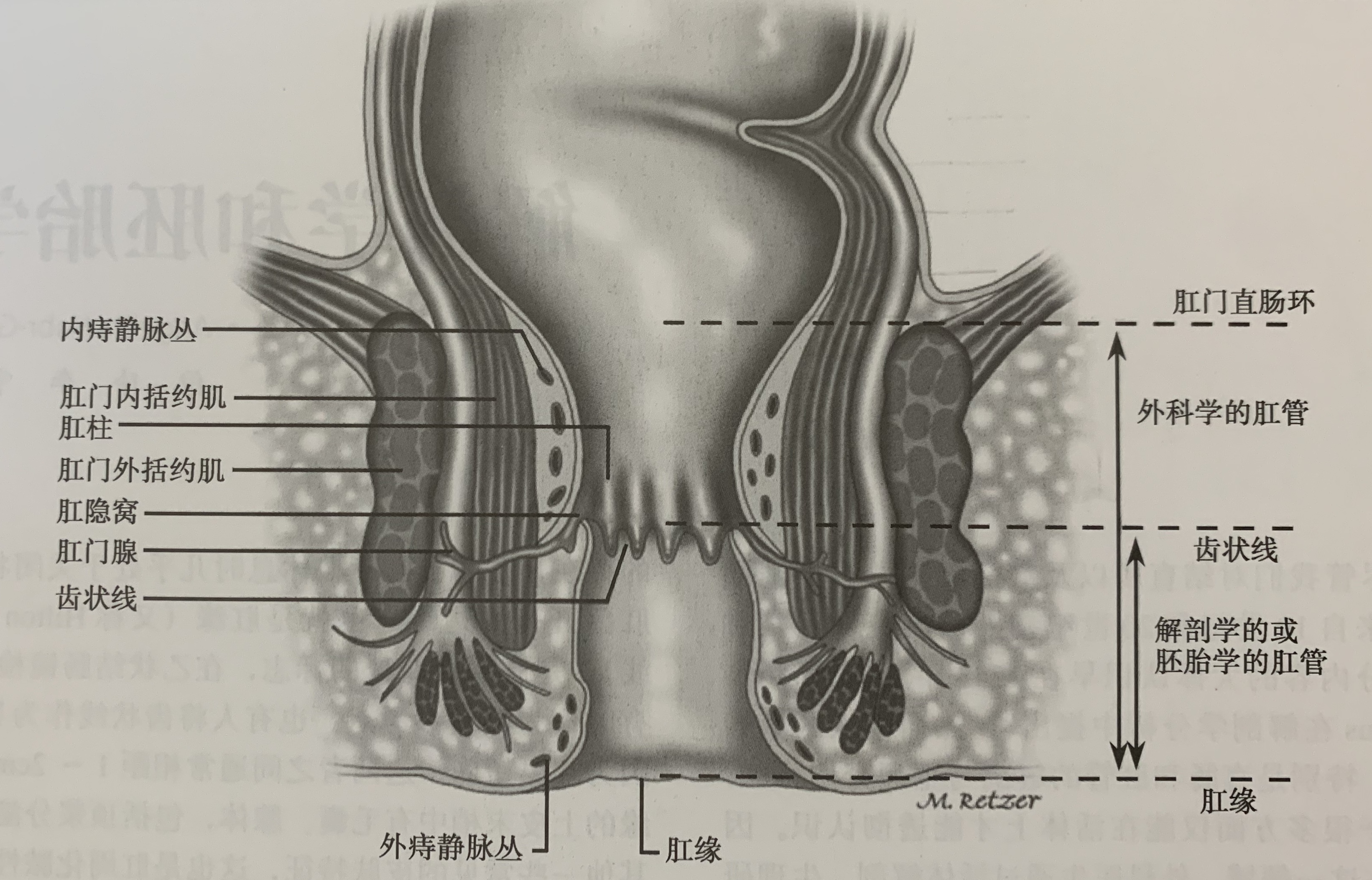
What is the anal canal?
The anal canal is the terminal part of the digestive tract, extending from the dentate line to the anal verge, measuring 3–4 cm in length (average 2.5 cm). The anal canal is divided into the anatomical anal canal and the surgical anal canal. The former refers to the part below the dentate line to the anal verge, while the latter extends from the upper edge of the anorectal muscular ring to the anal verge, approximately 1.5 cm above the dentate line.
Is hypertrophic anal papilla common?
The occurrence rate of anal papillae is 13%–47%, with most people not having them. Hypertrophic anal papilla develops due to chronic inflammatory stimulation in the anal canal, forming gradually. Thus, its incidence is relatively low.
Who is prone to hypertrophic anal papilla?
Individuals with frequent loose stools, proctitis, or chronic anal fissures are more likely to develop hypertrophic anal papilla.
Which department should be consulted for hypertrophic anal papilla?
Patients with hypertrophic anal papilla should visit the proctology or general surgery department.
SYMPTOMS
What are the symptoms of hypertrophic anal papillae?
- Patients with hypertrophic anal papillae may experience a foreign body sensation or discomfort in the anus.
- If the anal papillae are excessively enlarged, patients may feel a protrusion outside the anus during bowel movements. Smaller anal papillae may retract on their own after defecation, while larger ones may require manual assistance to be pushed back into the anus. Failure to reposition them promptly can lead to anal edema, swelling, and pain.
- When the swollen anal papillae are irritated or ulcerated, they may increase anal gland secretion, causing moisture and itching around the anus.
What serious consequences can hypertrophic anal papillae cause?
Hypertrophic anal papillae have the potential to become malignant, which could be life-threatening. Even without malignancy, significant discomfort from the foreign body sensation or frequent prolapse outside the anus may result in incomplete cleaning after bowel movements and perianal moisture, severely affecting the patient's quality of life.
What symptoms should raise suspicion of hypertrophic anal papillae?
If a patient experiences a foreign body sensation inside the anus, or if a firm, hypertrophic mass is detected near the dentate line during a digital rectal exam, or if there is a protrusion during bowel movements, hypertrophic anal papillae should be suspected.
CAUSES
What causes hypertrophy of anal papillae?
Hypertrophy of anal papillae is mainly caused by various inflammations and injuries. When there is inflammation, injury, or long-term chronic irritation in the anal canal or lower rectum, the anal papillae gradually proliferate and hypertrophy, such as anal cryptitis, anal canalitis, old anal fissures, etc., which can all lead to hypertrophy of anal papillae.
Which groups are prone to hypertrophy of anal papillae?
People who frequently suffer from diarrhea or constipation, as well as those with conditions like anal cryptitis, anal canalitis, or old anal fissures, are more susceptible to hypertrophy of anal papillae.
DIAGNOSIS
What tests can diagnose hypertrophic anal papillae?
Digital rectal examination and anoscopy can provide a clear diagnosis. Digital rectal examination determines texture by touch—whether it is hard or soft—while anoscopy visually assesses whether it resembles anal papillae. Combining both examinations enhances diagnostic accuracy. Digital rectal examination alone provides only a preliminary judgment, but pairing it with anoscopy ensures a more definitive diagnosis.
Can hypertrophic anal papillae become malignant? How should this be determined?
Hypertrophic anal papillae have the potential to become cancerous, though the incidence is low. A definitive diagnosis can only be confirmed through pathological examination after surgical removal.
Which diseases are easily confused with hypertrophic anal papillae? How can they be distinguished?
Hypertrophic anal papillae are often confused with rectal polyps and internal hemorrhoids because all three occur near the dentate line and may prolapse during bowel movements. However, there are clear distinctions:
- Hypertrophic anal papillae: Located at the dentate line, covered by skin (transitional epithelium), smooth surface, white or pale red in color, rarely bleed, firm on palpation, and often multiple.
- Rectal polyps: Located above the dentate line, mostly in the rectal ampulla, covered by mucosa, dark red in color, prone to bleeding, soft on palpation, and usually single.
- Internal hemorrhoids: If the hemorrhoid is large, it may prolapse during bowel movements and be mistaken for hypertrophic anal papillae. However, hemorrhoids are soft in texture and often accompanied by bright red blood during defecation.
How can hypertrophic anal papillae be detected early?
When anal papillae are small, they typically cause no discomfort. Only when they grow larger do they cause a foreign body sensation or prolapse outside the anus. Therefore, for early detection, digital rectal examination and anoscopy are recommended.
TREATMENT
What are the treatment options for hypertrophic anal papillae?
Non-surgical treatments for hypertrophic anal papillae are ineffective, and surgical removal is required. Treatment methods include direct surgical excision or ligation with silk thread for脱落.
- If hypertrophic anal papillae prolapse outside the anus or cause discomfort due to a foreign body sensation, affecting daily life, surgical treatment should be considered.
- If hypertrophic anal papillae cause no discomfort, surgery may be temporarily unnecessary, but annual follow-up examinations are recommended.
What are the potential risks of surgery for hypertrophic anal papillae?
Surgery for hypertrophic anal papillae is a routine minor outpatient procedure. Postoperative bleeding is possible but occurs very rarely, with minimal risk.
Can hypertrophic anal papillae be cured? What is the cure standard? What is the cure rate?
After surgical removal, the hypertrophic anal papillae are eliminated, achieving a cure with a 100% success rate.
Can hypertrophic anal papillae recur after surgery? How likely is recurrence?
The removed anal papillae will not recur. However, since anal papillae are often multiple, other smaller papillae may enlarge due to inflammation or other stimuli, leading to new cases of hypertrophy.
DIET & LIFESTYLE
What should patients with hypertrophic anal papillae pay attention to in their daily lives to reduce the recurrence rate?
To reduce recurrence, patients with hypertrophic anal papillae should maintain a light diet, eat more vegetables and fruits, drink plenty of water, keep stools soft and smooth, and avoid constipation or diarrhea. If suffering from conditions like proctitis or anal fissures, active treatment is necessary.
Do patients with hypertrophic anal papillae need follow-up examinations after treatment?
After the removal of hypertrophic anal papillae, follow-up examinations are generally unnecessary. If discomfort occurs post-surgery, an anoscopy may be performed.
PREVENTION
How to Prevent Hypertrophy of Anal Papilla?
Not everyone has anal papillae, with an occurrence rate of 13%–47%. Those without anal papillae will not experience hypertrophy of anal papillae.
For individuals with anal papillae, maintaining perianal hygiene in daily life is essential. Actively treating perianal diseases such as proctitis and anal fissures can reduce inflammatory stimulation in the rectal and anal regions, thereby preventing hypertrophy of anal papillae.
How Can Patients with Hypertrophy of Anal Papilla Prevent Further Progression?
For patients with hypertrophy of anal papillae, surgical removal is generally recommended. Maintaining cleanliness in the rectal and anal areas, avoiding diarrhea or constipation, and actively treating perianal diseases like proctitis and anal fissures can help reduce local inflammatory stimulation.